Digestion 101: A North to South Process
As we continue more south in digestion, after first the brain and the mouth and then the stomach we move onto the accessory organs, the pancreas, liver and gallbladder
As we move further south from the stomach, while the small intestines are next in line for the food, but we first take a small pause/detour to discuss “the accessory organs of digestion”. The pancreas, liver and gallbladder, each play a very important role in the digestive process and each can be affected with their own dysfunction as well.
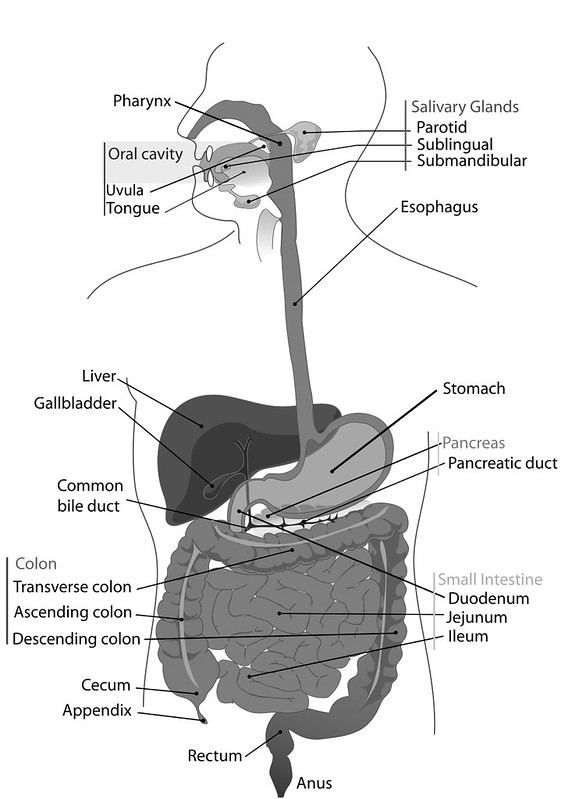
The stomach, small intestines and large intestines are all part of the system of digestion we call “the alimentary canal”, “the gut tube” or “digestive tube”. Between each of these organs we have valves or sphincters that keep the food where it is supposed to be and move it along when the time and the environment is right. These accessory organs are not a part of this tube or system but they play a major role in the process.
There is a synergistic and symbiotic relationship with the small intestines and these accessory organs, so we will discuss first how these play a role before we move into the function of the rest of the GI tract.
The duodenum is the start of the small intestine, but it almost acts more as part of the stomach, in it’s roles of breaking things down further playing a larger part in the process of digestion, vs the rest of the small intestine being less of a digestive organ and more about absorption or assimilation.
See Part One: The Brain and The Mouth
THE PANCREAS, GALLBLADDER AND LIVER:
How It’s Supposed to Work
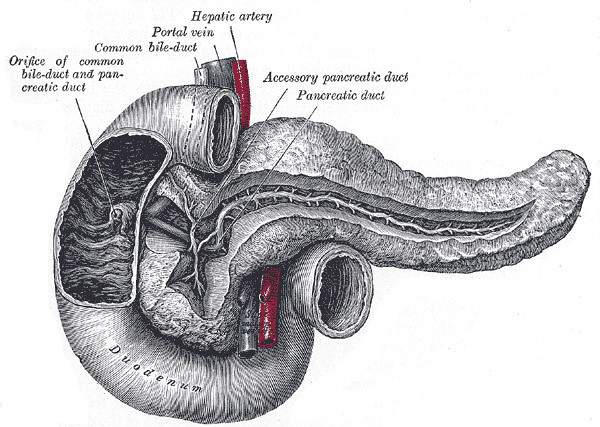
When the pH of the chyme (the digested food moving from the stomach into the small intestines) is in it’s normal range, 1.5 – 3.0 , which we talked about in the stomach post. This is very acidic and necessary to the stomach performing it’s duties. As it hits the pyloric valve and into the duodenum with it’s proper pH, this is where the roles of the accessory organs come into play. This highly acidic chyme is what triggers these functions.
The duodenum no longer wants this highly acidic chyme and in order for the enzymes to work correctly it has to take that chyme to a neutral pH of 7.0. This happens by way of sodium bicarbonate, which is released by the pancreas to alkalinize the chyme. This release of sodium bicarbonate is signaled by secretin, a hormone released by the small intestines, which as you might have already guessed, is triggered by the (proper) acidic level of the chyme, that pH of 1.3 – 5. (Ahem, here is that reminder to look north, if the stomach isn’t producing proper HCl, then none of this will function properly, either!!)
The sodium bicarbonate comes and floods the chyme until it reaches neutral, a pH of 7. From there the pancreas then knows that it should send in the digestive juices and enzymes, also stimulated by the secretin, to complete the chemical digestion of carbohydrates, proteins and fats with proteases, amylases and lipases.
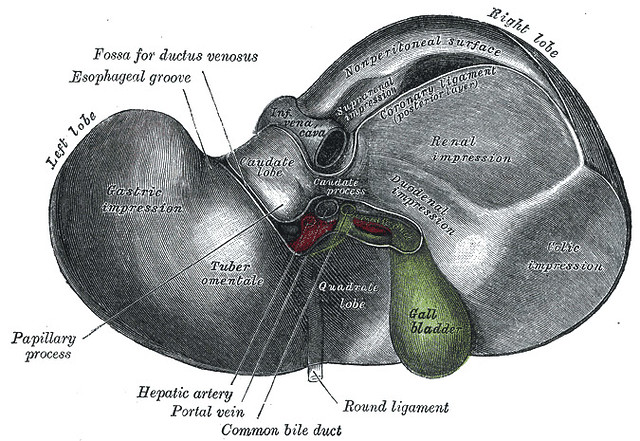
Concurrently another hormone, cholecystokinin (or CCK) is also stimulated by the small intestines. Unlike the bicarbonate signaled by the low pH, CCK is actually signaled by the presence of fat in the duodenum. When the body perceives the fat in the chyme in the duodenum, it then produces the CCK which sends a signal up to the liver/gallbladder. If the gallbladder is faithfully collecting and storing bile, which is constantly being produced in the liver, the CCK causes the gallbladder to squeeze and contract, releasing bile down the common bile duct and into the duodenum.
Bile is imperative to emulsifying and absorbing fats. Fat globules need to be emulsified to be properly digested and assimilated. At the same time, pancreatic lipase (enzymes) come in further break down the emulsified fats and it takes them and transports them to the lymphatics, to the liver and throughout the body.
By the time the chyme leaves the duodenum to head into the small intestines:
- carbohydrates are broken down into glucose molecules
- proteins have been broken down into amino acids and polypeptides
- fats are broken down into fatty acids and glycerol molecules and they move into the jejunum
Once the chyme has been alkalinized and broken down, it can move into the other parts of the small intestines, which we will cover in the next post, all about the small intestines.
What Can Go Wrong:
Improper pH Means the Functions of the Pancreas Will Not be Signaled
Without the proper pH 1.5 – 3 due to lack of hydrochloric acid in the stomach, due to diet, stress or due to the presence of antacids, etc – the chyme will not properly move into the duodenum in the time that it should, so when it finally does continue on, after wreaking havoc in the stomach, it will likely have larger food particles, which should have been properly digested in the stomach but could not be. The chyme will also not be at the proper pH, for example if the chyme is at a pH of 5 (rather than the necessary 1.5 – 3) because of the lack of HCl, this means the hormone secretin won’t be released to trigger the sodium bicarbonate by the pancreas to properly neutralize the chyme, nor will the pancreatic enzymes be released.
Without the sodium bicarbonate to alkalinize the chyme and raise the pH, we would still be at this hypothetical acidic level of 5. The duodenum does not want this at a 5, it wants it at 7, so that the rest of the functions can continue. This acidic chyme over time, not getting properly neutralized, can effectively burn the mucosal lining which can lead to duodenal ulcers. Additionally, without those pancreatic enzymes being triggered to release, this means incomplete digestion, undigested proteins, which means intestinal issues, which we will talk about in the upcoming post on the small intestine.
Gallbladder Dysfunction
Due to poor quality fats, lack of fat or a low fat diet, the gallbladder can dysfunction, in several different ways. Fats are digested by the bile salts and pancreatic lipase in the duodenum. Fat in the chyme stimulates the release of CCK which stimulates the gallbladder to release bile. A low fat diet will not trigger the release of bile causing the bile, which is constantly being produced by the liver and stored in the gallbladder, to go unused. This leads to stasis, the gallbladder will then fill up and the bile can get old/viscous. Bad fats, will also cause the bile to become viscous. Not only can this lead to gall stones, which bring a whole bunch of their own problems, but the gallbladder will attempt to contract in the presence of fat, to release the bile to help in digestion, but it won’t be able to, because of this viscous bile. Without bile, we are unable to absorb fats, these undigested fat globules that cannot be digested will rancidify in the colon, which leads to digestive issues and this will also stress out and further toxify the liver, it will exacerbate any existing biliary dysfunction and leave you fatty acid deficient. Gallbladder dysfunction can also lead to pancreatitis and other issues. Conventional medicine at many of these points typically suggest removing the gallbladder, as many claim it’s not really necessary, and as you can see this is simply not the case. Literally to me, this is highly prevalent medical procedure is one of the saddest and most highly avoidable medical interventions. The gallbladder can be saved!
Additionally, there is a misconception that someone with gallbladder issues and pain, should be on a low fat diet and as you can see, this is actually so far from the truth and that very diet will actually exacerbate this problem.
WHAT YOU CAN DO
ALWAYS Look North.
Start with Part 1, the brain and the mouth (read about what can go wrong and what you can do). Eating in a calm, parasympathetic state is imperative to the digestive process being properly activated. Start here with these very simple steps.
After practicing these mindful eating habits, look next at the stomach, be sure that you are producing enough HCl. This acidic environment is important to properly activating these accessory organs to properly do their job, to release the necessary hormones, which signals the release of enzymes, bile, etc.
High Quality Fat at Every Meal
Make sure you are eating, high quality, fat with every meal. The presence of fat triggers the small intestines to release the hormone CCK which is necessary to signal the gallbladder to release bile. (read above under dysfunction what happens when this doesn’t occur.) Adding healthy, high quality fats from avocados, grass-fed meats, wild caught fish, pasture-raised eggs, grass-fed butter, high quality, non-hydrogenated or overly refined oils, nuts, seeds, etc – this is such a simple change. Again this simple dietary adjustment can possibly save you from chronic gallbladder dysfunction, gall stones, sluggish gallbladder as well as issues further south, if your fats aren’t being properly broken down and eventually assimilated.
Additionally, if you have already had your gallbladder removed, I suggest speaking to your health care practitioner about supplementing with bile salts to replace what you are no longer receiving from the gallbladder, to aid in the proper digestion of your dietary fats.
Natural Enzyme Stimulation
As we talked about in the stomach post, warm lemon water, apple cider vinegar and digestive bitters can not only help to boost hydrochloric acid in your stomach but it also works to stimulate the rest of the digestive system to produce digestive enzymes and secrete bile which helps you digest your fats.
Warm Lemon Water:
At least 15 to 30 minutes ahead of a meal, slowly sip a mug of warm lemon water. This will stimulate the production of gastric juices. Use the juice of half of an organic lemon, in warm, but not hot, filtered water.
Apple Cider Vinegar:
Try one tablespoon right before a meal. If that is too harsh for you, you can also make a digestive tonic, with 1 teaspoon raw apple cider vinegar in ¼ to ½ cup warm water. Be sure to use real, unpasteurized apple cider vinegar.
Digestive Bitters:
Bitter flavors stimulate from the moment they hit our tongue, increasing the production of saliva and salivary amylase, it also triggers the stomach acid and enzymes, bile, hormones, etc. If the bitter taste is especially rare in your diet, your digestion will fire up with just a very small amount of the bitters. Take about ¼ teaspoon of bitters about 15 minutes before your meal. Make sure to use real bitters and not cocktail bitters, that may contain artificial flavors, preservatives, corn syrup, sweeteners or other junk. I recently discovered and love Urban Moonshine brand, made with with organic, gluten-free alcohol, and no GMOs- and they taste great.
NOTE: When traveling I suggest bringing along with an HCL supplement, digestive enzymes and a probiotic. These will help with arming your stomach to be prepared to deal with any unusual pathogens. This is especially important with international travel. We are already in a less than ideal state for digestion when traveling, we are out of control of our foods, stressed, etc. Take your support.
Digestive Enzyme Supplementation
Working with a naturopathic doctor, nutritional therapist, holistic health coach, etc – they can suggest a HCl and enzyme combination supplement if you need additional support. You will need to work with a practitioner to get your proper dosing, which is very unique to the individual and must be honored – for effective results and so as not to go too far.
————————————————————————
Digestion 101: A North to South Process
Part One: The Brain and The Mouth
Part Three: The Pancreas, Gallbladder and Liver
Part Four: The Small Intestine
Part Five: The Large Intestine
This post is for educational purposes only. This information is not intended to diagnose, treat, cure, or prevent any disease. Please always seek the advice of your holistic practitioner for contraindications with other medications. I am not able to recommend or prescribe for any medical conditions, without one-on-one consultation.




3 Responses
I have really been enjoying this series of posts. Thanks so much for the helpful information! I sometimes get overwhelmed in the aisles of Whole Foods when looking at things like probiotics and other supplements. You mention that when you travel you should take an HCL supplement, digestive enzymes and a probiotic: do you have a specific brand or type that you recommend or that you have found success with in the past? Thanks so much for the breakdown (pun intended).
What tips or suggestions would you give to someone who has had their gallbladder removed in terms of eating healthy?
You rock girl! This is awesome to have an understanding of how it all works and what our insides are all about because frankly it all seemed a little too confusing but you have made it very easy and clear.