-
Is Snacking Healthy? Should You Snack? + Smarter Snack Ideas
Is snacking healthy? Should you snack? If you find you are chronically grazing on many small meals throughout your day because of excessive hunger, you can likely blame imbalanced blood sugar and not eating for satiety. In this post we talk about snacking along with some healthy snack ideas for when a gap snack might be necessary.
Is Snacking Healthy? Should You Snack?
Let’s talk about snacks baby. Let’s talk about you and me. Let’s talk about all the good things and the bad things, that may be. Let’s talk about snacks! hahah. Sorry. I digress. Seriously though. Determining what to eat is challenging enough of a question, but add to that, the question of when and how often to eat – this adds a whole new additional layer of unanswered inquiries and confusion for many.
Smaller More Frequent Meals Helps Boost Metabolism, Right?
While convention nutritional advice long touted 5-6 small meals throughout the day as a means to increase your metabolism and encourage fat loss, this antiquated approach doesn’t look at the full scope of our day and what is actually happening in the body with every snack or small meal. For so long, many “experts” believed the idea that many small meals is theoretically “stoking the metabolic fire,” while less frequent meals “slow your metabolism.” The thought process was that eating many small meals keeps your metabolism plugging away at a high rate for the entire day, helping you burn more fat. Conversely, it was thought that going too long between meals slows down your metabolism, so that when you do eat, your body is sluggish to respond to the caloric load and you end up storing it as fat.
Sounds pretty smart, right? But, guess what, it’s just not true. There isn’t any science to support it or research that proves smaller, more frequent meals has any metabolic advantage.
What we do know, as research has shown, the more you eat the more insulin your body releases, and this constant output of insulin interrupts the intended flow of blood sugar.
With every meal there is a rise in our blood sugar (which is just the amount of free glucose in our bloodstream) then a release of insulin follows. With lots of small meals through the day that means a blood sugar rollercoaster of highs and lows that can cause additional cravings, fat storage, mood changes, irritability and more.
Besides that, with every meal or snack that we eat, our body has to begin the process of digestion, this takes energy and time, as your body is breaking down the food into usable molecules that are absorbed by the body and utilized appropriately. This process takes energy away from other repairs and tasks your body should be doing. Anything we eat that the body cannot absorb or use in some capacity is then stored as fat. Whenever we snack this stops the process of our body using stored body fat in between meals.
The goal is to instead build a day with more steady blood sugar by getting enough fat and protein at every meal to reach satiety and not solely relying on refined starchy carbs and sugar for quick hits.
-
5 Mealtime Tips to Improve Digestion
Digestive dysfunction is easily the most common chronic ailment I encounter working as a Nutritional Therapist. As a follow-up to my in-depth series Digestion 101, I wanted to offer five, simple actionable steps that you can take right away to immediately begin the improvement of your digestion.Digestive dysfunction can have many faces – gas, bloating, stomach aches, indigestion – we’ve all been there. Yes, there are plenty of quick-fix, short term “bandaid” approaches to managing the symptoms, I see so many people that often pop antacids, take anti-gas, diarrhea or constipation meds just to get through the day. Sadly this only manages the symptoms of a larger problem and more often than not the root cause of the dysfunction is left untreated and the problems still persist.
Rather than popping pills or difficult, unnatural approaches, here are 5 simple, meal-time tips to improve your digestion, naturally.
5 Mealtime Tips to Improve Digestion
-
4 Reasons to Avoid Vegetable and Seed Oils
4 Reasons to Avoid Vegetable Oils. Vegetable oils are NOT healthy! Read on to discover the 4 biggest reasons to avoid these terrifying, toxic fats!

On the regular I find myself saddened and unpleasantly surprised by the lack of easily accessible, reliable information and data concerning food, nutrition and health. Truthfully, looking back, it’s amazing how little I myself knew, before I started down this long, self-initiated, ongoing path of nutritional education and empowerment of the past 10+ years. I am often reminded these days that I live in a bubble of sorts, surrounding myself virtually and otherwise with bloggers, healers, nutritionists and content creators whose lifestyles mirror my own. Reading books, listening to podcasts and following doctors and researchers creating and sharing important information and research about health and nutrition. I tend to forget and maybe I even take for granted, how much I do know and often I find myself making sweeping assumptions that everyone else knows most of it, too. I know for so many of you this post and this information is old news, it’s a rerun, you’ve heard it before. But if this post reaches even one new person, if I can send my new nutritional clients, who are still cooking with vegetable oils, here to learn more, then it’s a success!
As I enter the homes of my nutritional clients, as well as my close friends and family members, the number one thing I see among their food choices, that I immediately want to remove from their pantries and toss aggressively into the garbage: is vegetable and seed oils. In my opinion, vegetable oils are far worse than any overly refined carbs, white sugar or high fructose corn syrup. This deadly, Frankenstein-eque, lab-created “food” (if you can even call it that) is wreaking more havoc on people’s health than possibly anything else and sadly it’s being overlooked by so many. Much of this comes from Western medical practitioners who are woefully uneducated in nutrition or those whose nutritional education is sorely dated, built on antiquated and debunked health myths of previous generations. Or maybe it’s the fact that big food industry in our country has a large stake in corn and soy production and these have become, by far, the cheapest crops we are growing, thanks to government subsidies. Take a look at most packaged and processed foods and I can almost guarantee you will find one or both of these foods somewhere on the label.
The edible oil industry in our country, “Big Ag” and their marketing “geniuses” sought to demonize tropical oils and other saturated fats and in turn, in the same breath to promote their own vegetable oils, like corn and soybean oil. This great movement toward the excessive use of polyunsaturated fats and the demonization of saturated fats came with the advent of the “Lipid Hypothesis” — which featured fraudulent research made by a terrible scientist named Ancel Keys who made unsubstantiated claims that saturated fat and cholesterol were the cause of heart disease and ignored research and data that didn’t support his argument. We can see how well all that has gone!
The fats used in this study were hydrogenated, processed fats, known to be extremely irritating to the body, particularly the vascular system. Cholesterol acts as a healing agent to repair and protect the arteries and veins. Therefore, the more irritation, the more cholesterol will mobilize to save the day! Research now shows us that dietary cholesterol intake has VERY LITTLE to do with over all cholesterol levels, so this part of the theory was off target as well. Today, the Lipid Hypothesis continues to be promoted by most medical professionals and pharmaceutical companies, as well as the modern food processing giants, who profit from such flawed research. Saturated fatty acids from healthy sources nourish the vascular system, enhance immune function, protect the liver from certain toxins (including alcohol), aid in calcium absorption, and increase cellular membrane integrity. Keep in mind that heart disease was considered a rare condition before the 1920’s, but spiked dramatically from 1910 to 1970 as Americans began consuming less saturated animal fats and increasing amounts of vegetable fats in the form of margarine, shortening and adulterated, refined oils of all types. Our not-so-distant ancestors consumed healthy sources of saturated fats each and every day with no adverse health effects whatsoever! 1Fats: Safer Choices for Your Frying Pan and Your Health By Caroline Barringer, CHFS, NTP
After going through the Nutritional Therapy program at the NTA to become a certified Nutritional Therapy Practitioner I have found myself more inspired than ever to want to help people, to share what I know and to do whatever I can to help make a change in our health, our very broken food system and to empower people to make the very best choices for themselves and their families. So let’s start with one of the most important topics: 4 Reasons to Avoid Vegetable and Seed Oils!
What are Vegetable Oils?
Vegetable oils are oils that are extracted from seeds, germs or beans, such as corn, sunflower, safflower, soybean, or rapeseed (canola oil), etc. Non existent until the early-1900’s, vegetable oils are one of the most unnatural “foods” you can find. Vegetable oils are PUFAs, which stands for Poly-Unsaturated Fatty Acid. In chemical terms, that means that the fatty acid has more than one (poly) double bond in the carbon chain. They’re unsaturated because they’re missing out on what saturated fatty acid has — hydrogen atoms. In a sense, that makes the bonds sort of incomplete. So, imagine a chain of links that are sort of missing a joint or two, on each and every link — it wouldn’t be very strong or stable. These messed up and broken chains make for highly unstable fats that are prone to oxidation in the presence of heat and light, during cooking, sitting on the shelf in the grocery store or in your kitchen pantry and even in your body and they turn rancid, which our body reacts terribly to. Our body attempts to respond to and neutralize the oxidization by utilizing its stores of antioxidants. This oxidization process causes cell mutation, which we see in chronic inflammation, the source of most of the worst illness plaguing our society, cancer, heart disease, etc.
It’s really pretty simple. Because of their instability, and the negative effects on the body’s systems these oils have in excess, PUFA are just plain bad.
The most common vegetable oils on the market are:
- soybean oil
- canola oil (rapeseed oil)
- sunflower oil
- corn oil
- cottonseed oil
- “vegetable” oil
- safflower oil
- peanut oil
- grapeseeed oil
- rice bran oil
- margarine
- shortening (made from above oils)
- fake butter or spreadable butter-type spreads (I Can’t Believe it’s Not Butter, Earth Balance, Smart Balance)
Thankfully less and less people are cooking with these oils at home these days, however unfortunately it’s still not enough to just not buy these cooking oils at the store. Be aware that many/most processed foods contain these oils so you have to be sure to read labels. Salad dressings, condiments like mayo, sauces, crackers, cookies, chips… check your ingredients. You can also bet that most restaurants are cooking in vegetable oils, because they are so cheap! Unless a restaurant specifically states otherwise, their fried foods are all cooked in soybean, cottonseed or some other highly toxic vegetable oil.
(Note the term “vegetable oil” does NOT apply to healthy plant oils like olive oil or coconut oil, which are extremely healthful)
4 Reasons to Avoid Vegetable Oils
References
1. ↑ Fats: Safer Choices for Your Frying Pan and Your Health By Caroline Barringer, CHFS, NTP -
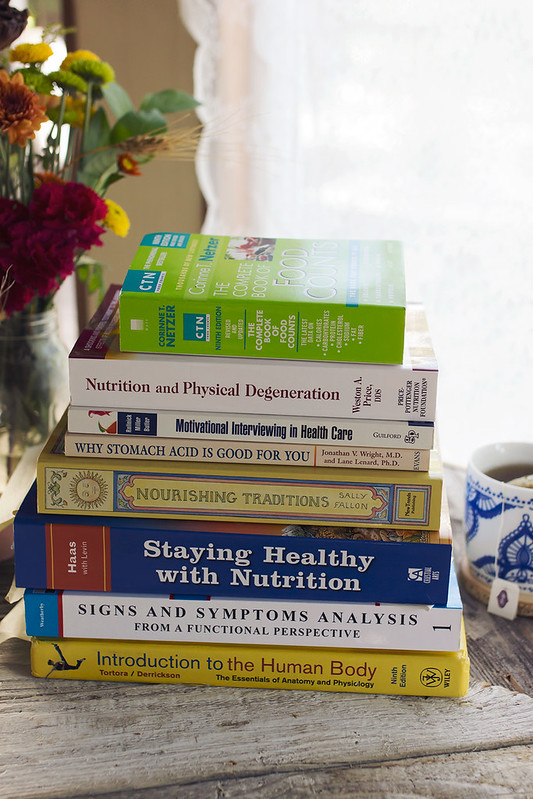
My Path to Becoming a Certified Nutritional Therapy Practitioner – Months 7 – 9
If you keep up with me on social media you may probably already know that I not only finished the Nutritional Therapy Association Program in June and graduated, but I totally aced my exams and I am now an officially certified Nutritional Therapy Practitioner. Woohoo!! I have also already begun seeing a small amount of clients. It’s been a whirlwind of a year and I went ahead and just hit the ground running since graduation – then I realized that I never updated and finalized this series. This is the last post chronically my journey to becoming a Certified Nutritional Therapy Practitioner with the Nutritional Therapy Association, speaking to the final 3 months of the program. I plan to, from here, create one final post that is an FAQ of sorts, that I will continue to update as people reach out to me with questions about my experiences, since sadly I don’t always have the time to reply to each and every email, as much as I would love to. If you have any questions in regards to the program or my certification, please feel free to leave a note here in the comments or reach out via email.
My Path to Becoming a Certified Nutritional Therapy Practitioner – Months 7, 8 & 9
This post continues to share my journey of becoming a Nutritional Therapist with the Nutritional Therapy Association, covering Months 7, 8, and 9, April, May and June. To read more about how I came to selecting this program and to read about Month 1 of the program, see my first post. To read about months 2 and 3, month 4 and months 5 & 6 you can read more at those respected links.
-
Digestion 101: A North to South Process // Part 5: The Large Intestine
Digestion 101: A North to South Process
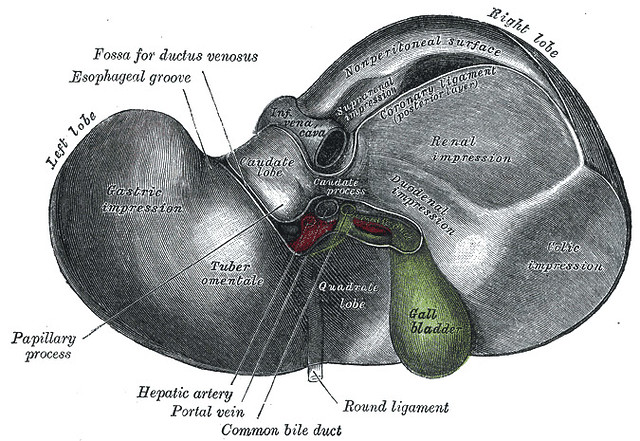
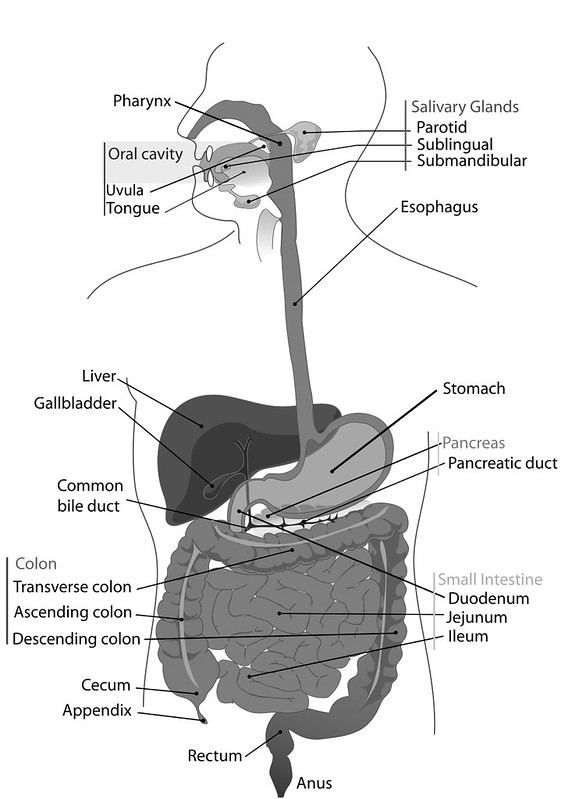
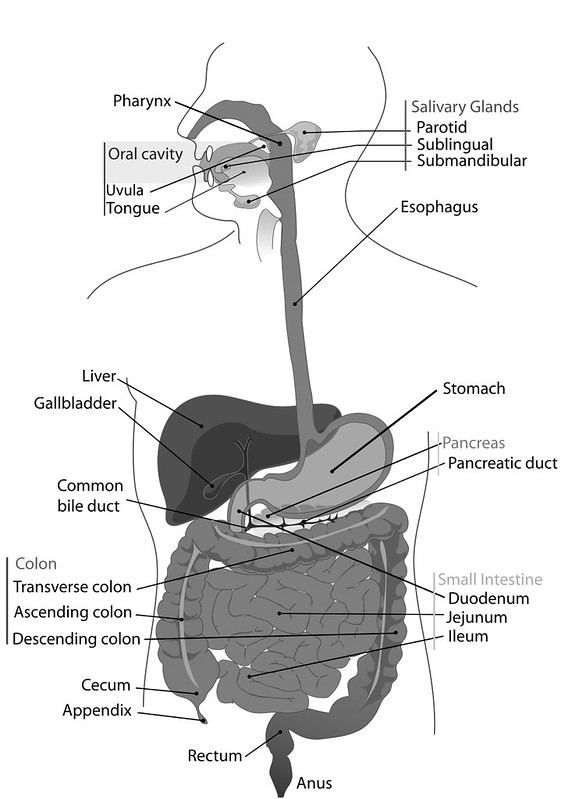
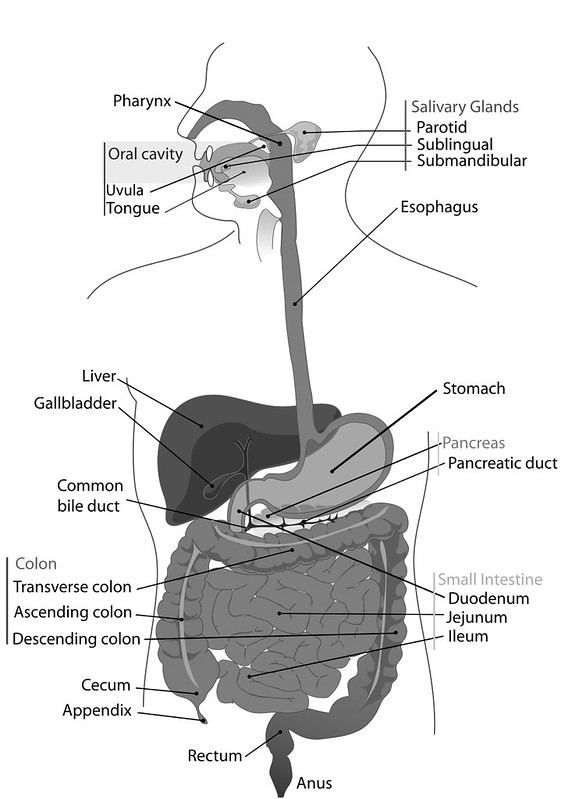
Here we are, at the end of the road. The large intestine is the final step in the process of digestion. By this point you probably more than understand the concept of digestion being a north to south process. We have talked about it at length starting first the brain and the mouth, and the importance of being in a parasympathetic state and properly chewing your foods, then of course the stomach and the dire need for proper hydrochloric acid production, how the accessory organs, the pancreas, liver and gallbladder continue the process of digestion, releasing bile, enzymes, various hormones and allowing the small intestines to finish digestion but more importantly do it’s very important job of assimilating nutrients and finally last but not least, the large intestine.
See Part One: The Brain and The Mouth
See Part Three: The Accessory Organs: Pancreas, Gallbladder and Liver
See Part Four: The Small Intestine
How it Should Work
The large intestine, or the bowel, is compromised of 3 sections, the cecum, colon and the rectum. The leftover chyme from the small intestines, passes through the illeocecal valve and first into the ascending colon. At this point in a healthy digestive system, what is left as chyme (the digested food) after the small intestines, is indigestible fibers, lots of water, sloughed off cells and bile. The large intestine is all about absorption and recycling.
As in the esophagus and the small intestine, the contents of the large intestine are pushed forward by a sequence of muscular contractions called peristalsis (a type of motility or muscular movement). After passing through the illececal valve the remains travels from the ascending colon, across the transverse colon where waste forms, into the descending colon, to the sigmoid colon and then the stool moves out of the body.
-
My Path to Becoming a Certified Nutritional Therapy Practitioner – Months 5 & 6
My Path to Becoming a Certified Nutritional Therapy Practitioner – Months 5 & 6
This post continues to share my journey of becoming a Nutritional Therapist with the Nutritional Therapy Association, covering Months 5 and 6, February and March. To read more about how I came to selecting this program and to read about Month 1 of the program, see my first post. To read about months 2 and 3, read my second post and to read about month 4 read my third post.
Month 5
The fifth month of this program was by far the most challenging for me, the content continued to roll in and simultaneously we were preparing for our mid-term examinations, the first weekend of March. Being a self proclaimed perfectionist I wanted to ace the exams, while of course, I also really wanted all of the content to be very clear to me. That meant lots of studying, lots of flash cards, memorizing and generally freaking myself out! It worked! I missed one tiny little thing on my written mid-term examination and had 1/2 point taken off on my functional evaluation practical exam. ACED!
Month 6
The first weekend of month 6 was our second workshop weekend, 4 long days. First we had our exams and then we spent the remainder of the weekend going over the content we had covered since our last meeting as well as continuing to practice the functional evaluations (you can read more about function evaluations here). After the workshop weekend we were on term break for just under 1 month. Read the rest of this entry »
-
Digestion 101: A North to South Process // Part 4: The Small Intestine
Digestion 101: A North to South Process
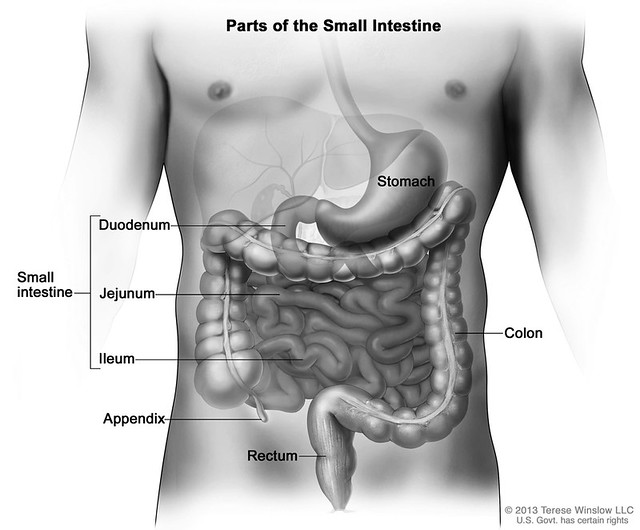
As we continue more south in digestion, after first the brain and the mouth, then the stomach we move from the first part of the small intestines, the duodenum and it’s interaction with the accessory organs, the pancreas, liver and gallbladder and into the function of the small intestine.
After we leave the duodenum, the small intestine is less about the actual process of digestion, from a sense of breaking down the food we eat and it is more about the assimilation and absorption of nutrients.
The first part of the small intestines, the duodenum, acts more as a part of the stomach than the small intestine and the jejunum, ileum and villi are responsible for assimilation.
See Part One: The Brain and The Mouth
See Part Three: The Accessory Organs: Pancreas, Gallbladder and Liver
How it Should WorkThe small intestines have a dual role as an organ and a gland.
As we talked about in the previous post, The Accessory Organs – The Pancreas, Gallbladder and Liver, the small intestine releases mucous to keep things moving and it also releases two hormones: secretin and cholecystokinin.
Secretin stimulates the pancreas to release bicarbonate to lower the pH of the chyme and pancreatic juice. The CCK stimulates the gallbladder to release bile (to read more about these processes please see post #3).
By the time that the chyme has left the duodenum, thanks to the processes of the accessory organs, the chyme should be almost entirely digested.
- The carbohydrates have been broken down into glucose molecules
- Proteins are broken down into amino acids and polypeptides
- Fats are broke down into fatty acids and glycerol molecules
Peristalsis, a series of wave-like muscle contractions moves these absorbable molecules into the jejunum and the ileum, the middle and end parts of the intestine.
Within the small intestines, we have millions of villi, tiny finger-like projections that protrude from the epithelial lining of the small intestines. These villi and their microvilli absorb the nutrient molecules directly into the bloodstream, where they are carried throughout the entire body.
-
Digestion 101: A North to South Process // Part 3: The Accessory Organs – Pancreas, Gallbladder and Liver
Digestion 101: A North to South Process
As we continue more south in digestion, after first the brain and the mouth and then the stomach we move onto the accessory organs, the pancreas, liver and gallbladder
As we move further south from the stomach, while the small intestines are next in line for the food, but we first take a small pause/detour to discuss “the accessory organs of digestion”. The pancreas, liver and gallbladder, each play a very important role in the digestive process and each can be affected with their own dysfunction as well.
The stomach, small intestines and large intestines are all part of the system of digestion we call “the alimentary canal”, “the gut tube” or “digestive tube”. Between each of these organs we have valves or sphincters that keep the food where it is supposed to be and move it along when the time and the environment is right. These accessory organs are not a part of this tube or system but they play a major role in the process.
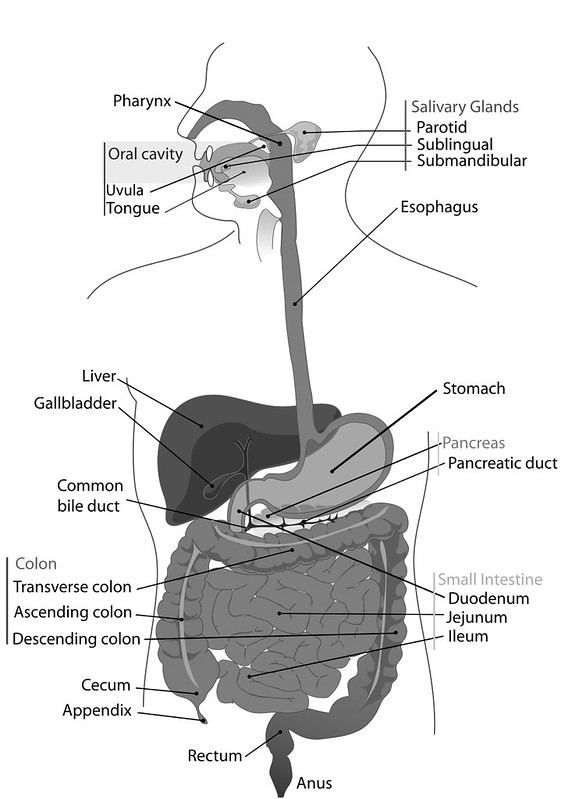
There is a synergistic and symbiotic relationship with the small intestines and these accessory organs, so we will discuss first how these play a role before we move into the function of the rest of the GI tract.
The duodenum is the start of the small intestine, but it almost acts more as part of the stomach, in it’s roles of breaking things down further playing a larger part in the process of digestion, vs the rest of the small intestine being less of a digestive organ and more about absorption or assimilation.
See Part One: The Brain and The Mouth
THE PANCREAS, GALLBLADDER AND LIVER:
How It’s Supposed to Work
When the pH of the chyme (the digested food moving from the stomach into the small intestines) is in it’s normal range, 1.5 – 3.0 , which we talked about in the stomach post. This is very acidic and necessary to the stomach performing it’s duties. As it hits the pyloric valve and into the duodenum with it’s proper pH, this is where the roles of the accessory organs come into play. This highly acidic chyme is what triggers these functions.
The duodenum no longer wants this highly acidic chyme and in order for the enzymes to work correctly it has to take that chyme to a neutral pH of 7.0. This happens by way of sodium bicarbonate, which is released by the pancreas to alkalinize the chyme. This release of sodium bicarbonate is signaled by secretin, a hormone released by the small intestines, which as you might have already guessed, is triggered by the (proper) acidic level of the chyme, that pH of 1.3 – 5. (Ahem, here is that reminder to look north, if the stomach isn’t producing proper HCl, then none of this will function properly, either!!)
-
Digestion 101: A North to South Process // Part 2: The Stomach
Digestion 101: A North to South Process
As we continue more south in digestion, after the brain and the mouth, next up we have the stomach. Before we get started, I wanted to remind you that you will constantly hear me reiterate as we go through this step-by-step process to “always look north” and I want you to truly understand what this means, exactly. I am referring to the fact that often times dysfunction that presents itself from further down the line, is actually due to a malfunction more north. For example, as you will read about in this second post and as we talked about briefly in the first, (the brain and the mouth), if you are eating in a stressful state and your body doesn’t make the necessary switch to that parasympathetic mode (rest and digest), then before your stomach ever had a chance to function properly, the brain basically threw it under the bus. So, while the symptoms may present themselves in the stomach (or even further south) it may not make sense to supplement, treat or approach the symptoms specifically until we instead move more north to investigate if these malfunctions are treatable with just some simple lifestyle and mindset shifts.
This is not at all to say that all digestive dysfunction starts in the brain, that would make my job and my own healthy journey so much simpler. In fact, there are many reasons why dysfunction can exist, as you will see, but beginning the investigative process at the start, way up north, allows us to rule out the possible, more simple resolutions before we move deeper and into more challenging treatments.
See Part One: The Brain and The Mouth
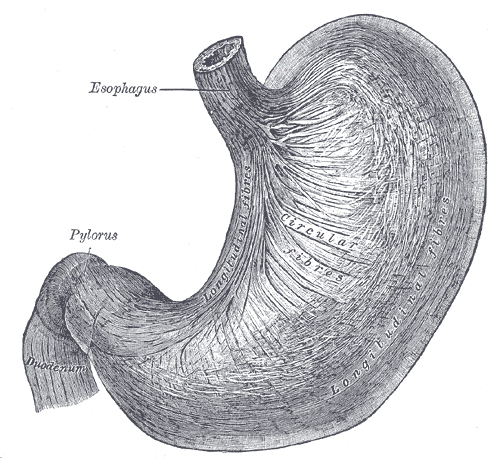
THE STOMACH:
How it’s Supposed to Work
After we chew our food, it turns into what we call a “bolus”. The bolus passes through the esophagus and the cardiac valve (the lower esophageal sphincter) and the bolus then enters our stomach, At this stage gastric juices are released. I like to think of the stomach as a blender. Mucous, pepsin and hydrochloric acid are all released for the “churning and burning” stage of digestion. Both mechanical and chemical breakdown happens at this stage.
The hydrochloric acid (HCl) being the most important of these gastric juices as it creates an acidic environment that disenfects the food and aids in the breakdown. Despite popular belief the stomach is absolutely meant to be acidic. In a healthy individual the pH of the stomach during digestion should drop to 1.5 to 3. We have a thick mucosal layer in our stomach, that acts as a barrier that protects the cells from the acid.
-
My Path to Becoming a Certified Nutritional Therapy Practitioner – Month 4
My Path to Becoming a Certified Nutritional Therapy Practitioner – Month 4
This post continues to share my journey of becoming a Nutritional Therapist with the Nutritional Therapy Association, covering Month 4, January. To read more about how I came to selecting this program and to read about Month 1 of the program, see my first post. To read about months 2 and 3, read my second post.
Month 4
After our first workshop weekend and the holiday break, we hit the ground running at the start of January. We dove straight into Mineral Balance and then Hydration, the final two modules focused on the foundations. The foundations being, Digestion, Blood Sugar Regular Regulation, Fatty Acids, Mineral Balance and Hydration and of course, a properly prepared nutrient-dense, whole food diet. It was nice to finish with hydration, really honing in the classic “last but not least” cliché.
As we have continued to submerge ourselves into the content with the Nutritional Therapy Program, especially the foundations, I am continuing to connect deeply with the NTA’s individualistic approach to nutrition. Honoring that we are all bio-chemical individuals, means that there is no one catch-all diet, plan or protocol for every person. We are all very different. There are certainly constants and research that suggests specific nutritional approaches to be ideal, such as the avoidance of refined sugars, processed foods, hydrogenate oils, etc. As my intuition has always directed me to suggesting that people “nourish their own individuality”, this program really supports my personal approach. It feels good to feel validated and to continue to hone my skills in approaching food, nutrition, and overall health and wellness in this manner. I love that this program teaches a very foundational and functional approach to nutrition, not relying solely on on specific diet or slapping supplements on symptoms, especially those associated with the consequences, as a bandaid! This approach is not just how I live my own life, it is what I feel called to encourage others to do as well! I want to help people find their inner guiding voice and couple that with an arsenal of nutritional knowledge, to be able to intuitively navigate their way towards healing.
I am also continuously grateful for the virtual platform that the NTA program is built on. I have discovered, that I learn so much more effectively when I am able to take in the content at my own speed, when it fits best into my life, vs. the structure of a timed class-setting. I also love that in addition to a virtual class setting, with multiple platforms to reach out to each other, there are three times throughout the program where we gather to have in-person workshop weekends, where we can connect with our fellow students, instructors and previous students, which really gives me something to look forward to.
-
My Path to Becoming a Certified Nutritional Therapy Practitioner – Months 2 & 3
My Path to Becoming a Certified Nutritional Therapy Practitioner – Months 2 & 3
This post continues to share my journey of becoming a Nutritional Therapist with the Nutritional Therapy Association. To read more about how I came to selecting this program and to read about Month 1 of the program, see my first post.
Months 2 & 3
I am combining months 2 & 3 together, as month 2 (November) was a regular, in-session month but at start of month 3 we had our first intensive in-person workshop weekend, followed by our holiday break.
The intensity and speed at which we were covering the first modules in month 1, has certainly calmed down a bit and with me finally catching up to my classmates (and our curriculum calendar), I am feeling much less pressure. I feel like I can breath and I can really let the content sit with me and permeate a bit more. For what it’s worth, the intensity I am speaking about, these are all things our instructors advised us of, going into the program. So I was certainly aware of this fact from the start and I wasn’t alone in feeling that way, I am sure. The content and reading materials are already starting to click quicker as new topics arise, pulling in previous content that we covered.
Most exciting about these past two months, was our first in-person workshop weekend, where we had the opportunity to meet our fellow classmates, as well as go over the content in person and ask questions of our instructors. Additionally we further honed our skills of client interviewing, analyzing Nutritional Assessment Questionnaires and Food Journals and making nutritional recommendations based on all of these tools and we learned and practiced the hands-on functional evaluation skills, for the modules we had already covered.
If you haven’t researched the NTA or if you’ve never worked with a Nutritional Therapy Practitioner you may not know what the terms Functional Evaluation and Lingual-Neuro Testing refer to:
Functional Evaluations are one of the Nutritional Therapy Practitioner tools for assessing a client’s health. Using the innate connection between nerve endings at skin level and the body’s internal organs, NTP’s can determine where dysfunction is occurring. Reflex points connect to the neuro-vascular and neuro-lymphatic pathways which surround every organ system in the body. When an organ is in stress, these pathways accumulate fluid around them (called venous or lymphatic congestion) to support healing. This congestion results in tenderness of the reflex points.
Lingual-Neuro Testing (LNT) is a valuable biofeedback tool that enables a health care provider to determine the usefulness of a nutritional supplement before it is dispensed to the client. LNT accesses the body’s innate ability to discriminate between what it needs, and what it does not need, in order to correct a specific problem–a weak organ or a nutritional deficiency, for example. This simple and effective technique makes the difference between a generic nutritional therapy plan and a personalized one.
-
My Path to Becoming a Certified Nutritional Therapy Practitioner – Month 1
My Path to Becoming a Certified Nutritional Therapy Practitioner
When I started Tasty Yummies, I was never inclined to create a journal of my own personal health journey, so I often refrain from getting super personal with my healing protocols and health challenges. I have consciously avoided flooding these pages with every discovery in my own ever-evolving health and dietary challenges or with every personal plan of action. Without any certification or credentials I often found myself feeling restricted from sharing too much of the self-initiated research I was doing, as I am hyper-aware of the barrage of claims made by bloggers without credible research or science to back it up. Mostly, I have always wanted Tasty Yummies to simply be a safe space to celebrate delicious, nourishing real food, and hopefully, a place to provide inspiration to empower others to take control of their health and to be open to discovering new foods themselves, whatever their restrictions or personal path may be. I have always sought to create a place to share my personal stories when appropriate and to cultivate a virtual connection among a supportive community of open-minded souls.
The fact remains however, that this website and my recipes wouldn’t exist without the many challenges I have experienced in my ongoing journey towards healing. Hidden within my own personal struggles emerged the desire to share, share, share! While none of my issues, in my mind, should be classified as “severe” or life threatening and while I don’t have epic before and after photos from an intense and acute health transformation, I would certainly still consider many of my health struggles to be chronic and some still unresolved. I am quite literally learning right along side many of you.
The Challenges.
As a child I dealt with a weakened immune system, allergies and asthma, migraines and troubled digestion. As life moved on, I discovered a severe gluten intolerance, and have now been gluten-free over 10 years – while this major dietary adjustment has certainly helped with some of these symptoms, I continued to suffer. In the early years of my adult life, even after going gluten-free, I struggled with weight gain and acne, chronic sinus infections, lack of energy and so much more, further adjusting of my diet has tackled much of this, but last year I was also diagnosed with IgA nephropathy, an autoimmune form of kidney disease. Consequently in the process of treating the kidney disease I also discovered through the help of my naturopathic doctor, that I was struggling with what we believe to be leaky gut, likely from the months of pharmaceuticals prescribed to me for the kidney disease. While I am still smack in the middle of this ongoing work to get my kidney disease in remission and my body to a point where I can feel good each and every day, I continue to share the recipes I am creating in my own kitchen, often part of my own healing path, in hopes that they may inspire some of you, within your own individual health journey, to feel less overwhelmed as you reconfigure your diets.
Why I want to Know More.
As a result of my own individual research and constant trials with nutrution, diet and supplementation, through my lens of seeing food as medicine and knowing that real food heals, I have come to the understanding that we are all bio-chemical individuals and there is no one protocol, diet or plan for all of us, there can’t be, we are all such beautiful and unique beings. I myself have always refrained from labeling my diet or pushing myself and this blog towards one specific label, as I find this to be ever-evolving process and for me, labeling my diet is not something I have ever felt called to. As with most everything in my life, my intuition instead constantly leads me towards balance and simplicity and learning to listen to my body’s innate cues, rather than adopting a static list of firm Do’s and Don’ts. I have found myself on a path of constant independent learning, research and exploration to find what works for me and through my search to help myself, I have oftentimes found I am able to help others as well, something I have learned I truly love and now feel called to do even more.
I have come to realize that in sharing my recipes, through instructing yoga, hosting retreats and teaching cooking demos, these are all amazing ways I am able share my passions and hopefully empower others to take control of their own health and their well being. But, I have been feeling that when it concerns food and our health, that I wanted to make an even bigger impact, I want to be able to host cooking demos and speak with conviction and credibility about how we can deal with chronic comprised digestion, blood sugar regulation issues and I want to share the precise scientific reasons why certain ingredients are making an appearance in my recipes. I want to be able to better respond to folks seeking to make recipes fat free and explain to them in a concise way, why it is so important to include healthy fat in our diet and the list really just goes on and on. Finally, I have met so many incredible, yet desperate people over the years looking for answers, I have many family members and friends that struggle with their health daily and I want to help however I can, anyone who comes to me inquiring. I want to crush these old, antiquated myths surrounding eating and our diets and reveal the truth about food and it’s healing powers.
All of this lead me to the Nutritional Therapy Association.
Why the Nutritional Therapy Association?: